Talking To Your Kids About Suicide

Suicide is a real risk for our youth, it remains the second leading cause of death for youth age 10-24 in the United States. It is very important for you to know that suicide isn’t about bad parenting! One of the simplest and most accurate definitions of suicide states that it is an alternative solution to a problem of intense emotional distress by someone whose problem-solving skills are impaired. There may be many reasons for the impairment, and being compromised mentally or emotionally is usually at the top of the list. Possibly more helpful to you right now than understanding the causes of suicide is outlining steps that may help you recognize if your child may be at risk – and what you can do about it.
Step 1: Keep your head out of the sand!
We know that it can be hard for any parent to acknowledge that their child may be struggling with something that’s beyond their capacity as a parent to fix; yet having thoughts about taking one’s life is one of those things that really requires professional intervention. Your part in this process is to pay attention to your child ‘s feelings and behavior, to ask about what concerns you, and, if necessary, get professional help. How do you do all that? Take a deep breath and read on.
Step 2: Recognize warning signs.
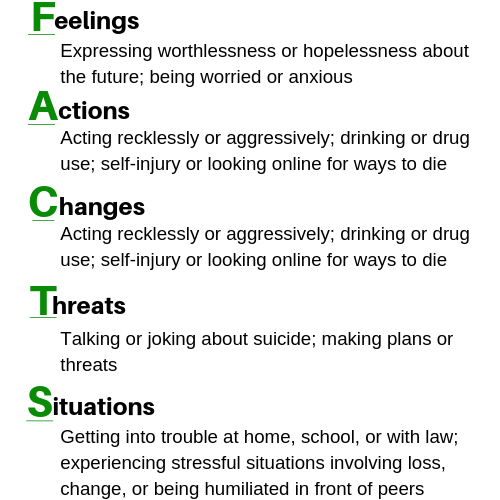
Take a look at the column to the right. This is a list of the more common warning signs we see in young people, organized under the acronym FACTS. As you read it you may find yourself wondering if these behaviors aren’t common in most adolescents. The answer of course may be ‘yes’, so we have to drill down a little farther. Think about this series of questions:
- How often have you noticed any of the FACTS? If you see more than one and you see them lasting at least two weeks, that may be a sign that they’re more serious than common adolescent behaviors. Be really concerned if you hear any talk or threats about suicide, especially if these are accompanied with changes in behavior or appearance. Remember, threats may be subtle: “I’ve changed my mind about college, I don’t want to go anymore”; “I’m tired of my friends; “There’s just no point…”.
- Are other people worried about your child? Sometimes your child’s friends, classmates or teachers may express concern about your child. Listen to what they say! They may be observing things that you don’t see and their perspective is important. Peers in particular are often the first to know when a friend seems different so don’t dismiss what they have to say.
Step 3: Ask questions and listen to the answers.
It’s really hard to hear a child tell you something that’s upsetting without trying to fix it. We live in a culture that values problem solving, so to simply listening and asking your child to tell you more about their distress can be extremely hard. The more information you have about what’s happening in their lives, the easier it will be to come up with an action plan.
- Remember: asking about suicide won’t plant the idea in your child’s head. There is a lot of evidence that shows asking about suicide can relieve the pressure that comes with keeping it as a secret. If you hear something from your child that really concerns you, try asking a question like:
“Sometimes when people feel the way you do, they think about taking their lives. I’m wondering if you’ve ever felt that way?”
- If you get a “yes”, simply say: TELL ME MORE. Your natural reaction, as we said before, will be to try to make those feelings go away, but catch yourself before you say something like: “you’ve been through harder stuff” or “you’re making this into a bigger problem than it really is”. Those responses may convince your child that you don’t want to hear what they have to say.
Step 4: Create an action plan.
There are two kinds of action plans: “urgent” and “wait and see”. Let’s review both.
- URGENT plans reflect your concern that your child may do something to harm him/herself in the near future. For example, if your child admits to thinking about suicide and having a plan, you need to act immediately to get what’s called a ‘risk assessment’ by a qualified mental health professional. If you’re not sure where to go to get that, you can reach out to the counselor at your child’s school for a recommendation or if you’re worried that there is an immediate risk to your child’s safety go to the nearest hospital emergency room that does risk screenings.
- WAIT AND SEE plans indicate you have some reason for concern but there doesn’t seem to be a need for immediate action. Your child may, for example, deny feeling suicidal or have reasonable explanations for the changes you’ve noticed. This doesn’t mean, however, that everything is okay. Keep your eyes open and perhaps pay a little more attention to your child. Run the situation by someone you trust- your physician, clergy member, school counselor- and get their input. When in doubt, getting a risk assessment may be the safest thing you can do for your child. While your child may not be suicidal, there may be other things going on that need your attention.
Step 5: Make your home safe.
If you have ANY worries about your child’s personal safety, even if they seem insignificant, take the precaution of removing lethal or potentially deadly things from your home until you are sure the crisis has passed. These include prescription or over the counter medications and firearms. This is a temporary measure that, again, reflects protection for your child when he/she may not be able to protect themselves.
Step 6: Realize you’re not alone!
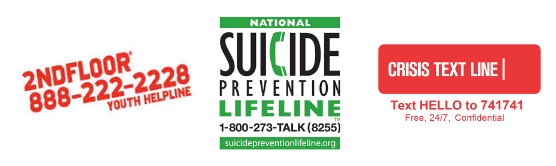
Worrying that your child may be thinking about suicide is probably one of the scariest thoughts you’ll ever have and you may need support to get some perspective. Many states have local hotline numbers where trained volunteers are available to help you sort through your feelings. If you have trouble locating a local number, give the National Suicide Prevention Lifeline a call…1-800-273-8255. When you dial this number, your call will be directed to a regional center close to where you live so you might even get the names of local resources to whom you can reach out.
We know this isn’t an easy conversation to have with anyone, especially your own child. However, being able to talk about their feelings or thoughts of suicide can be a relief to children who may be keeping it all bottled up. You can’t fix a problem you haven’t identified, and demonstrating that you’re willing to talk about difficult things like suicide may reassure your child that they can talk with you about any of their many challenges of adolescence. You CAN do it!!

